Purpose:
To guide therapists on the use of the Assessment / Plan to guide strong clinical documentation and justification of skilled therapy services that are reasonable and necessary.
Question Intent:
The Therapy Assessment / Plan section is intended to provide the interpretation of objective testing as well as the justification of why skilled therapy is reasonable and necessary for the patient at this time. It is important that these primary components are documented to support the patient’s need for skilled therapy services.
Per Medicare Benefit Policy Manual Chapter 7 - Home Health Services, the Therapy Assessment / Plan portion of our notes helps support that "the skilled services must also be reasonable and necessary to the treatment of the patient's illness or injury or to the restoration or maintenance of function affected by the patient's illness or injury. It is necessary to determine whether individual therapy services are skilled and whether, in view of the patient's overall condition, skilled management of the services provided is needed."
At Reassessment (at least every 30 days) timepoints therapy documentation supports continued payment based on a rationale that supports skill. Comparing current and prior levels with discussion to their relevance is a requirement both for CMS compliance and auditing bodies. Per the Medicare Benefit Policy Manual Chapter 7 - Home Health Services “At least once every 30 days, for each therapy discipline for which services are provided, a qualified therapist (instead of an assistant) must provide the ordered therapy service, functionally reassess the patient, and compare the resultant measurement to prior assessment measurements. The therapist must document in the clinical record the measurement results along with the therapist’s determination of the effectiveness of therapy, or lack thereof.”
Response – Specific Instructions:
- At Reassessment (33) visits the therapist will select Therapy Assess/Plan in their visit note. The initial question will determine the further questions that appear in the system. If the therapist selects CONTINUE SERVICES, the system will prompt for a free text question of the therapist's assessment followed by a therapy plan question. If the therapist chooses DISCONTINUE SERVICES, review the 33 Discharging Patient From Discipline for guidance. (NOTE - Therapists should ONLY discharge from a '33' service code if the circumstances leading to discharge occur during the Reassessment visit. If Therapist is aware of discharge prior to visit, the service code should be updated to the appropriate 18 or 19 service code prior to the in-person visit)
- If the plan is to CONTINUE SERVICES, the therapist will address the prompt below. Guidance is to separate your documentation into 2 paragraphs:
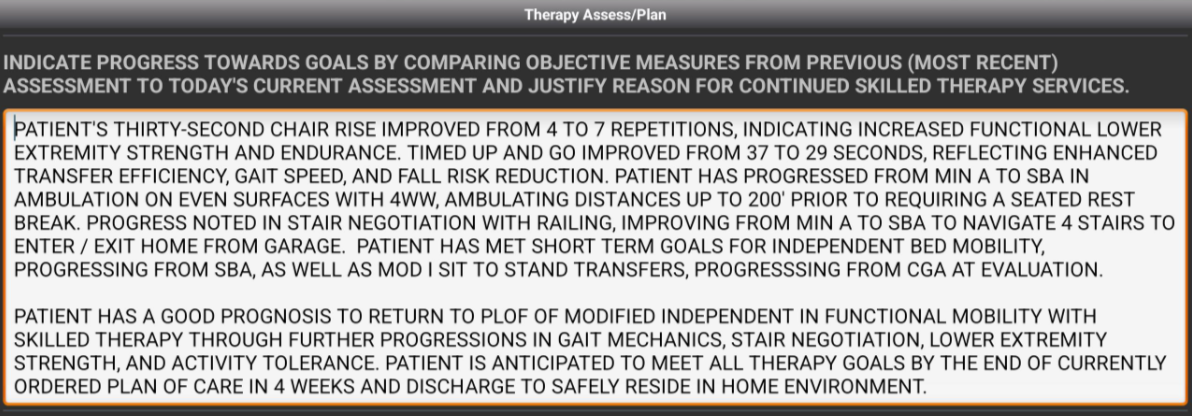
- First Paragraph - Comparison of objective measures (functional tests, functional independence measure scoring, etc) to prior assessment results. Be sure to document the results from the prior assessment visit to demonstrate improvements, or lack thereof.
- Second Paragraph - Make a case for why the patient will benefit from further skilled therapy, specific to your discipline. It is helpful to call out the patient's prognosis and what functional measures will objectively improve with further skilled therapy.
- Example:
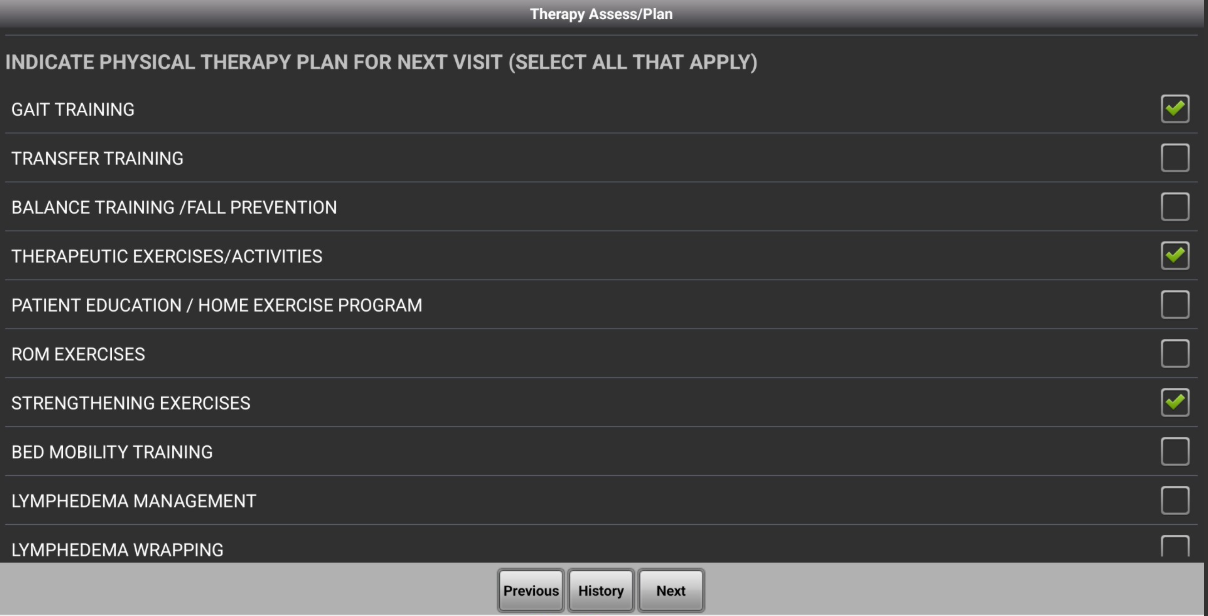
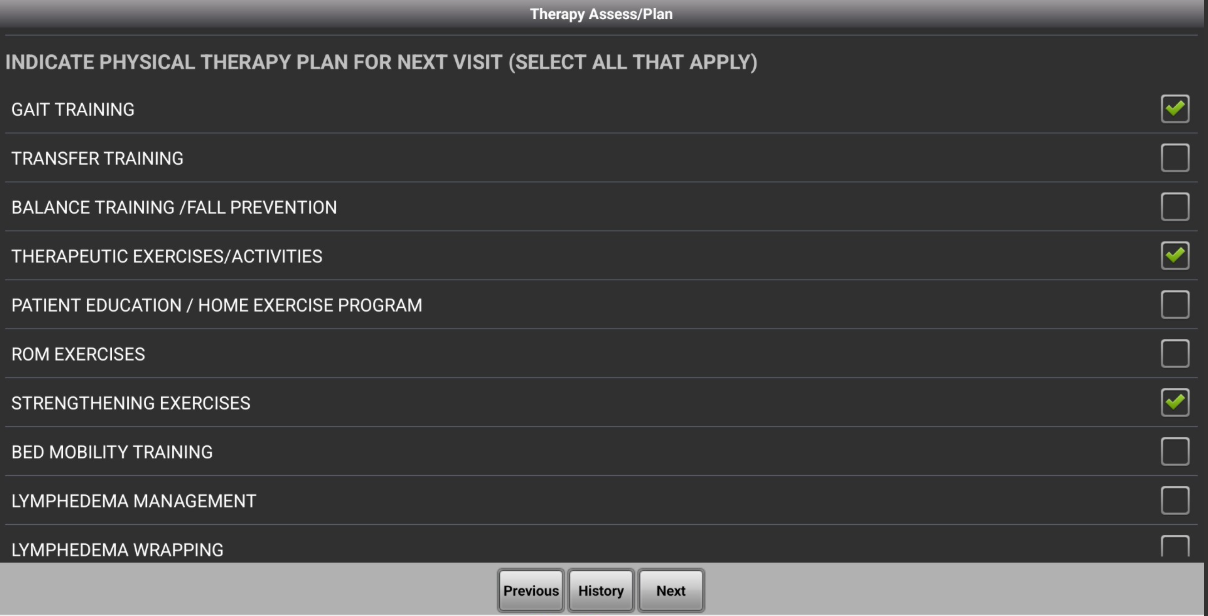
- Next, the Therapist will determine the plan for next visit by selecting the appropriate items in the list. Below is an example of the Physical Therapy list (each list is unique per discipline):
- The ‘plan’ is not an order. If you decide to provide a new intervention that was not in the original plan because of the reassessment findings you will need to complete a HH PointCare Plan of Care Update to create a new order for provider signature.