Purpose:
Notify patient/representative that have Medicare or Medicare advantage of an upcoming discharge to allow the patient the to appeal the discharge from agency.
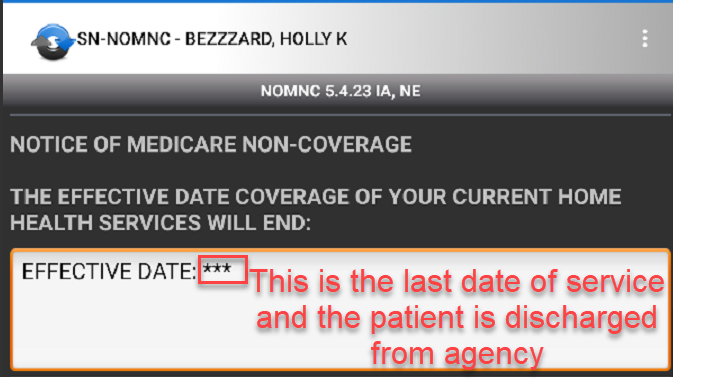
The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily.
Regulation:
Policy:
Education:
Process:
- Admission packet should include the paper NOMNC depending on type of Medicare insurance that should be added to the admission packet to ensure patient is given a paper copy for the Medicare insurance they have.
- A Buddy Code is needed to allow the NOMNC to be signed by patient/caregiver at the home visit.
- If arrived at home and Buddy code is not scheduled, contact office to add and then a sync to add NOMNC buddy code to rolling calendar and then another sync to accept will need to occur to fill out form.
- Review with client/representative at least 48 hours prior to discharge.
- NOTE: The paper NOMNC form will be reviewed with patient and the patient keeps this form with them for their records
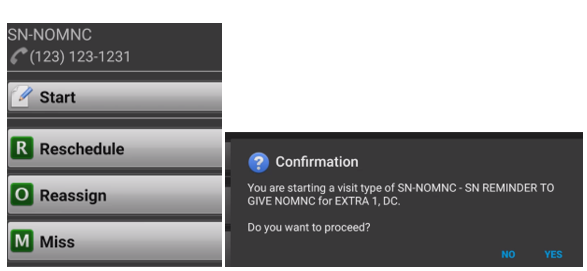
- Clinician will start, then confirm the appt for the NOMNC-
- Buddy code should be on the same day as the appt in home to review and sign the tablet to show proof of review.
- If Buddy code needs to be moved to a different day choose the reschedule option and perform a sync 2 times to allow to show up on rolling calendar.
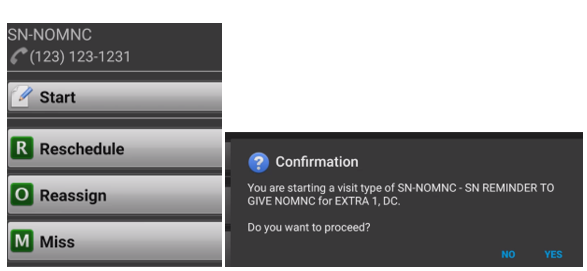
- If Buddy code needs to be moved to a different day choose the reschedule option and perform a sync 2 times to allow to show up on rolling calendar.
- Buddy code should be on the same day as the appt in home to review and sign the tablet to show proof of review.
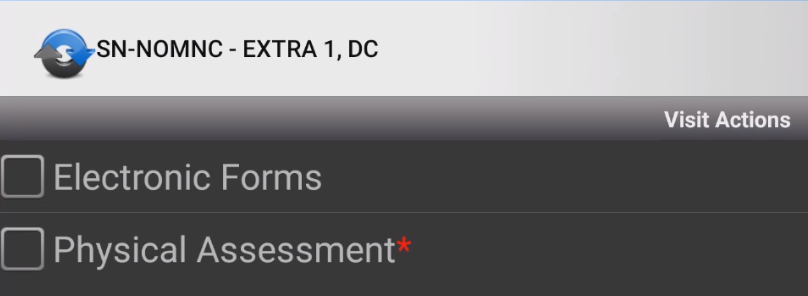
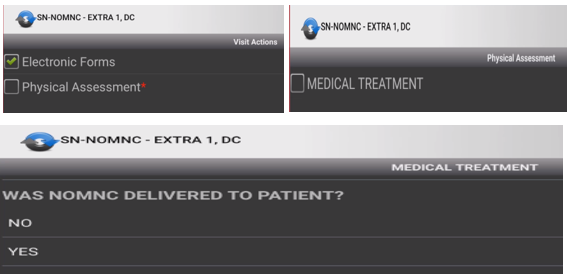
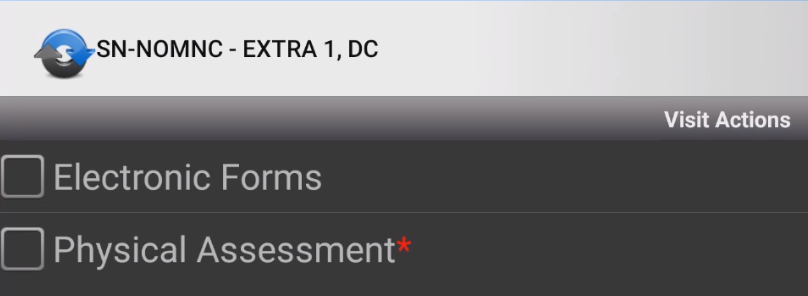
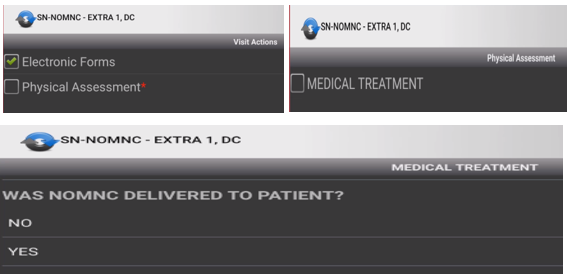
- Select Visit Actions to open up the NOMNC form.
- There will be 2 areas that will need to be completed
- Electronic Forms
- Physical assessment
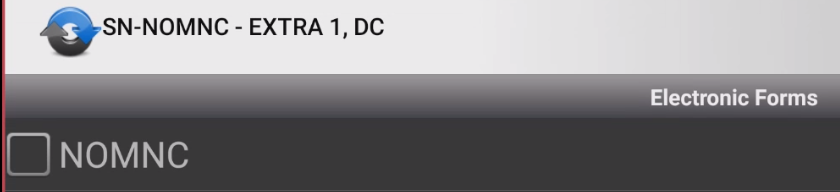
- Select Electron Forms and the NOMNC option will appear
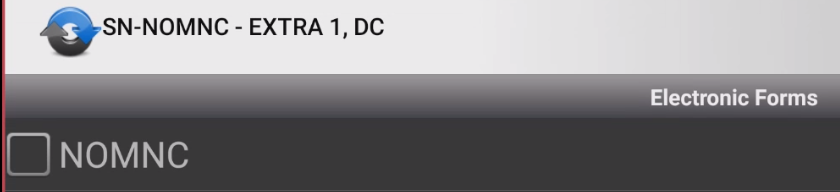
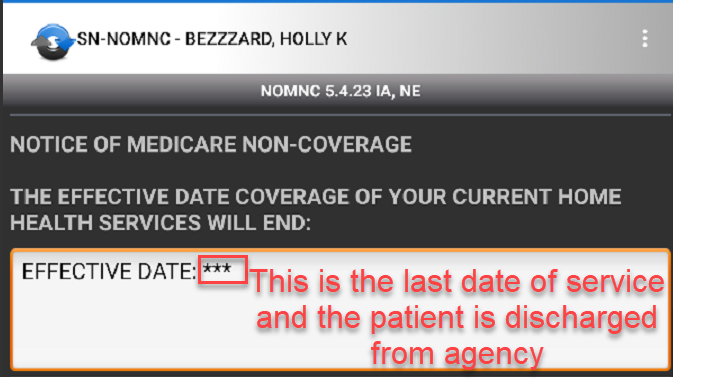
- The form will be an electronic version of the paper form in the patients home admission folder.
- Review the paper form with the patient and complete the required electronic form on tablet.
- The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily.
- The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily.
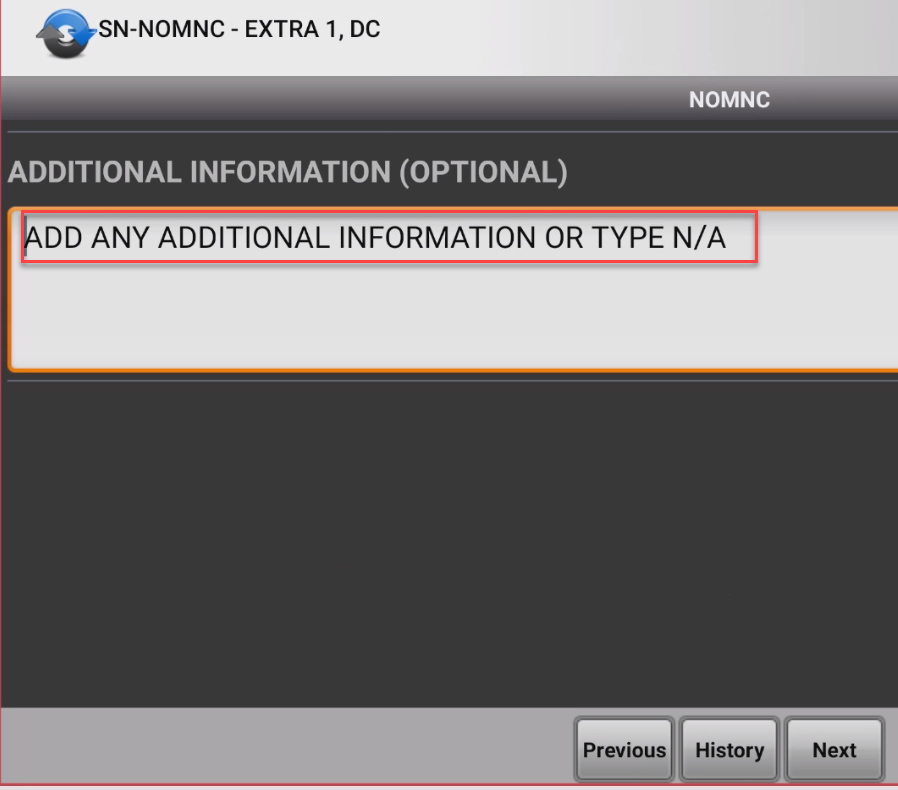
- Continue to click Next and scroll through form adding required text fields
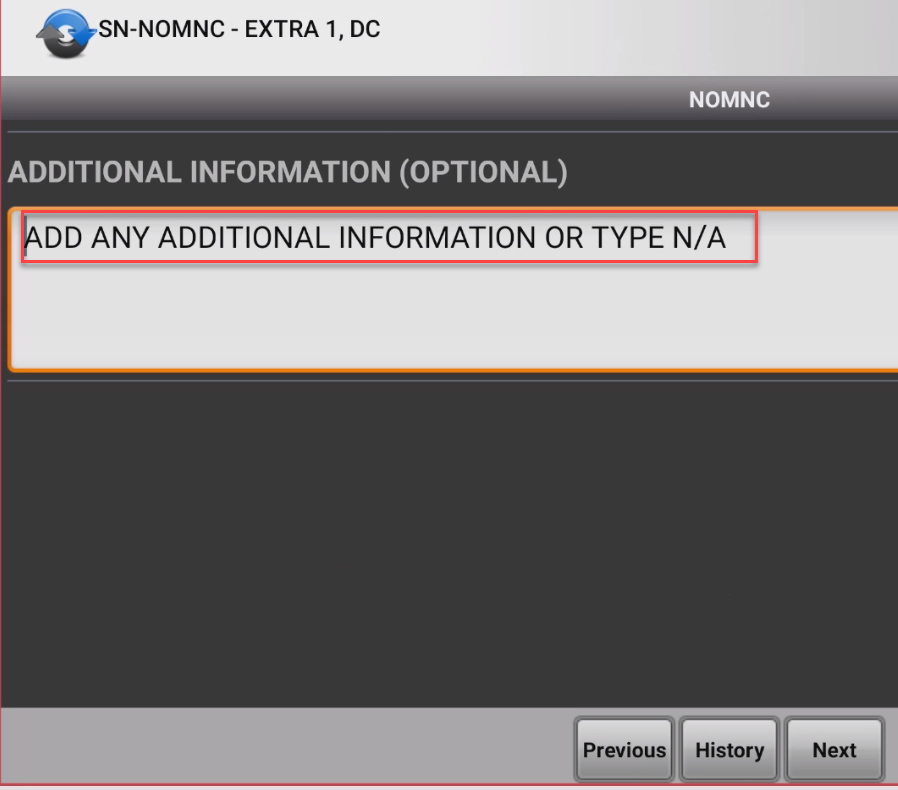
- If there is any additional information that would need to be added to the form, enter in this area or type N/A.
- Continue to hit next to move through form.
- When form is completed a green check mark will appear.
- Click Save

- Click Save
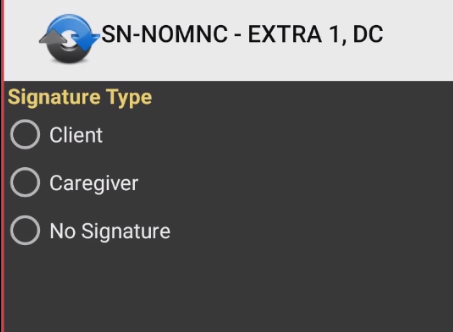
- A Signature should be obtained by the patient/caregiver
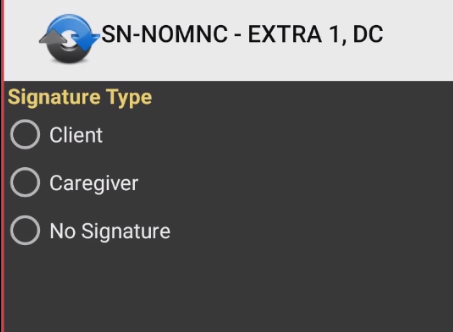
- Continue to hit next to move through form.
- The green check mark next to Electronic forms will show that this is completed and then the Physical Assessment will be selected to answer one question in Medical Treatment "Was NOMNC delivered to patient?"
- Select Yes
- Complete and Sync.
- Review the paper form with the patient and complete the required electronic form on tablet.
- There will be 2 areas that will need to be completed
- Notice Delivery to Representatives when not able to be at home visit to sign form on tablet.
- CMS requires that notification of changes in coverage for an institutionalized beneficiary/enrollee who is not competent be made to a representative. Notification to the representative may be problematic because that person may not be available in person to acknowledge receipt of the required notification. Providers are required to develop procedures to use when the beneficiary/enrollee is incapable or incompetent, and the provider cannot obtain the signature of the enrollee’s representative through direct personal contact. If the provider is personally unable to deliver a NOMNC to a person acting on behalf of an enrollee, then the provider should telephone the representative to advise him or her when the enrollee’s services are no longer covered.
- The date of the conversation is the date of the receipt of the notice. Confirm the telephone contact by written notice mailed on that same date. When direct phone contact cannot be made, send the notice to the representative by certified mail, return receipt requested. The date that someone at the representative’s address signs (or refuses to sign) the receipt is the date of receipt. Place a dated copy of the notice in the enrollee’s medical file. When notices are returned by the post office with no indication of a refusal date, then the enrollee’s liability starts on the second working day after the provider’s mailing date.
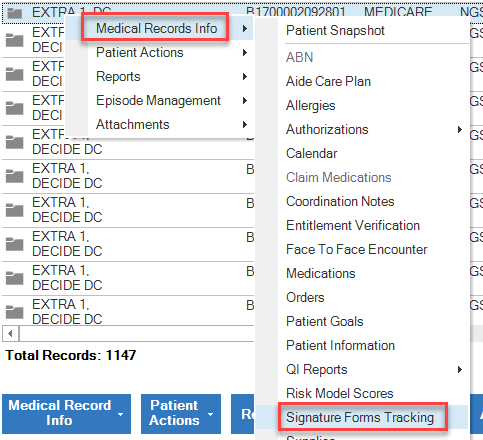
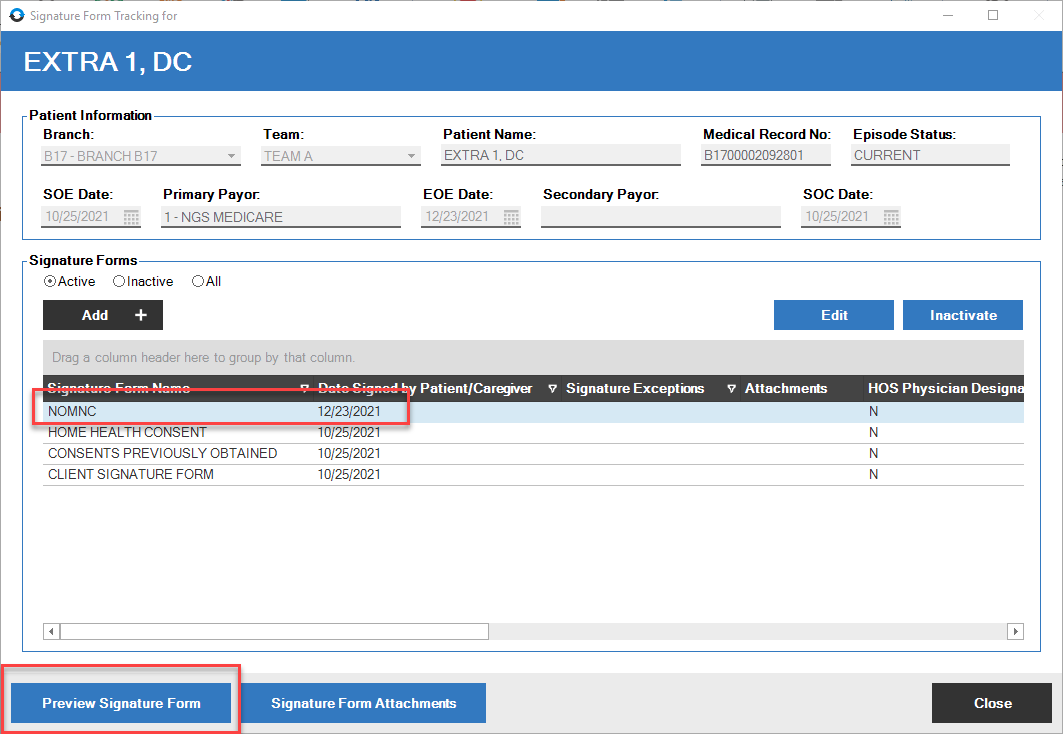
- To locate the NOMNC signed form.
- Right click on patient name in clinical input- select Medical Record, then select Signature forms tracking
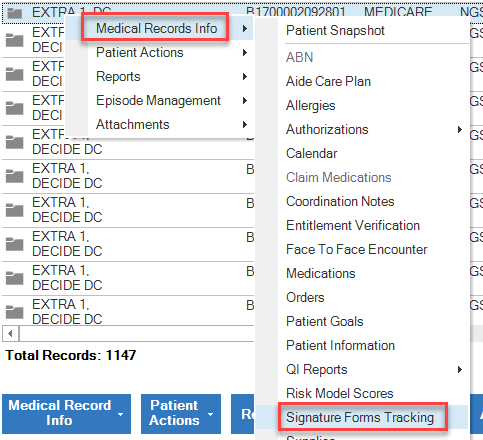
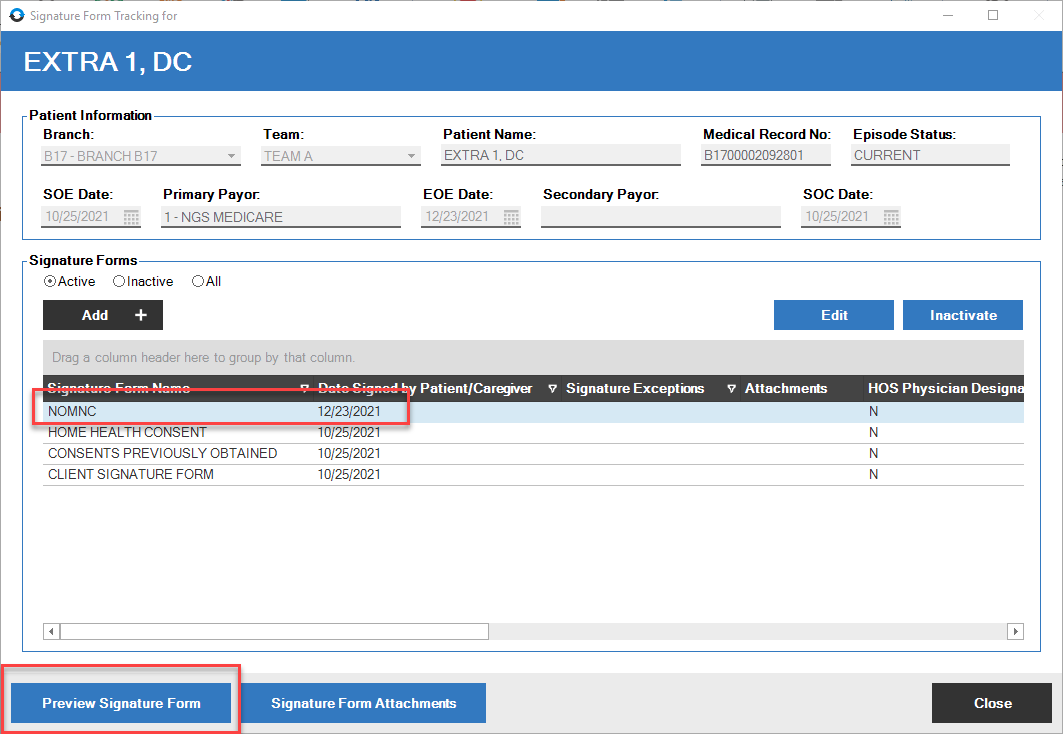
- Right click on patient name in clinical input- select Medical Record, then select Signature forms tracking