Purpose:
To guide therapists on the use of the Assessment / Plan to guide strong clinical documentation and justification of skilled therapy services that are reasonable and necessary.
Question Intent:
Per Medicare Benefit Policy Manual Chapter 7 - Home Health Services, 40.2.1 - General Principles Governing Reasonable and Necessary Physical Therapy, Speech-Language Pathology Services, and Occupational Therapy :
"Clinical notes should be written such that they adequately describe the reaction of a patient to his/her skilled care. Clinical notes should also provide a clear picture of the treatment, as well as “next steps” to be taken. Vague or subjective descriptions of the patient’s care should not be used. For example terminology such as the following would not adequately describe the need for skilled care:
• Patient tolerated treatment well
• Caregiver instructed in medication management
• Continue with POC
Objective measurements of physical outcomes of treatment should be provided and/or a clear description of the changed behaviors due to education programs should be recorded in order that all concerned can follow the results of the applied services."
Response – Specific Instructions:
- At Routine (11) visits each visit should indicate the patient's response to treatment as well as how the patient is progressing towards their goals. This documentation speaks to incremental gains from visit to visit or week to week as compared to a formal reassessment whish is longer in length and more thorough of the entire plan of care. Keep responses to routine visits concise and relevant to the day's visit.
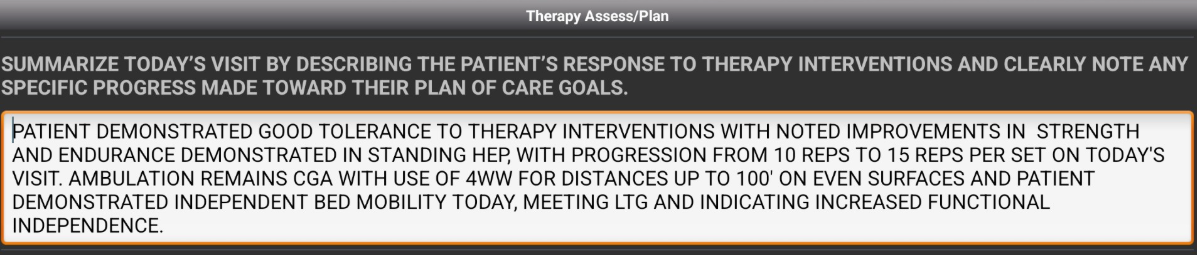
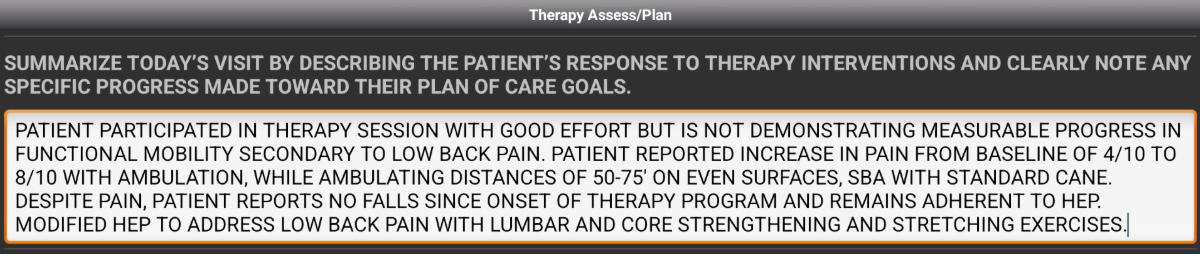
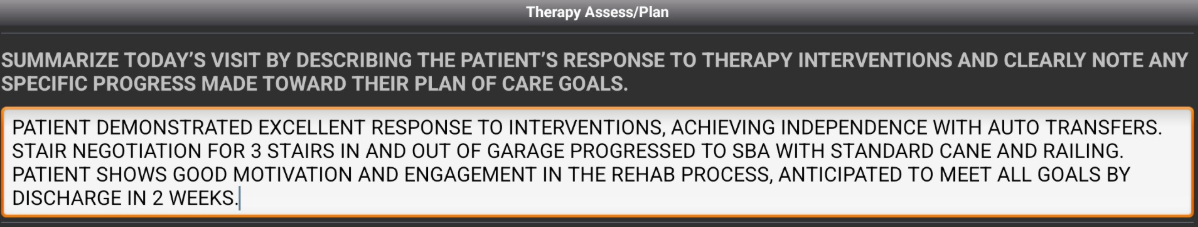
- Below you will find 3 examples of documentation that address both the patient's response to therapy interventions and progress toward goals.
- Lastly, you will indicate the continued therapy plan. Select from the drop downs the items that you plan to complete next session. The lists are discipline specific, and will vary for PT, OT, and ST notes. Below is an example for PT/PTA notes: