Purpose:
To guide therapists on the use of the Assessment / Plan on their discharge visit to guide strong clinical documentation and justification of skilled therapy services that are reasonable and necessary.
Question Intent:
The Therapy Assessment / Plan section is intended to provide the interpretation of objective testing as well as the justification of why skilled therapy services were necessary and the progress the patient made towards goals. It is important that these primary components are documented to support the patient’s need for skilled therapy services.
Per Medicare Benefit Policy Manual Chapter 7 - Home Health Services, the Therapy Assessment / Plan portion of our notes helps support that "the skilled services must also be reasonable and necessary to the treatment of the patient's illness or injury or to the restoration or maintenance of function affected by the patient's illness or injury. It is necessary to determine whether individual therapy services are skilled and whether, in view of the patient's overall condition, skilled management of the services provided is needed."
At Reassessment (at least every 30 days) timepoints therapy documentation supports continued payment based on a rationale that supports skill. Comparing current and prior levels with discussion to their relevance is a requirement both for CMS compliance and auditing bodies. Per the Medicare Benefit Policy Manual Chapter 7 - Home Health Services “At least once every 30 days, for each therapy discipline for which services are provided, a qualified therapist (instead of an assistant) must provide the ordered therapy service, functionally reassess the patient, and compare the resultant measurement to prior assessment measurements. The therapist must document in the clinical record the measurement results along with the therapist’s determination of the effectiveness of therapy, or lack thereof.”
Response – Specific Instructions:
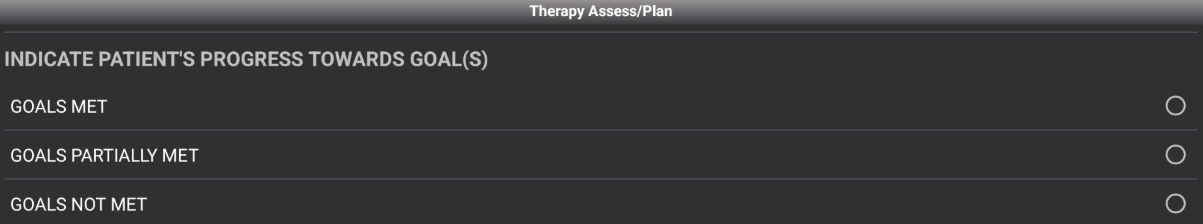
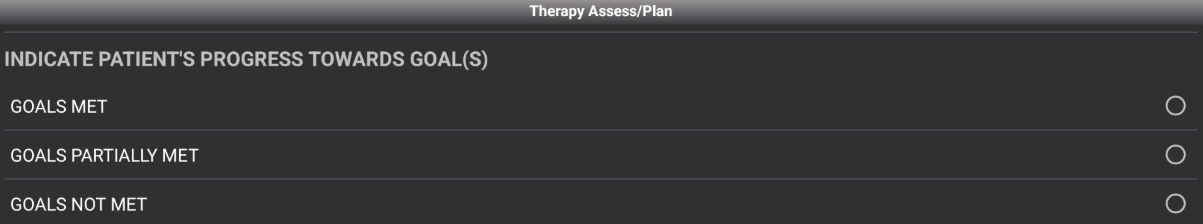
- At Discharge (19) or Agency Discharge (18) visits the therapist will select Therapy Assess/Plan in their visit note. They will first identify one of 3 options (GOALS MET, GOALS PARTIALLY MET, or GOALS NOT MET).
-
- NOTE - To view all goals in making this determination, the therapist should view Therapy Goals/Status as well as using the top right menu and going into Medical Records --> Order History to see all Goals written on the 485/Plan of Care.
-
- Once Progress Towards Goals is selected, a free text box will appear indicating DISCHARGE SUMMARY OF PATIENT'S FUNCTIONAL PROGRESS TOWARDS OUTCOMES AND GOALS. Here the therapist will address all goals objectively. An example where patient has met all goals is below:
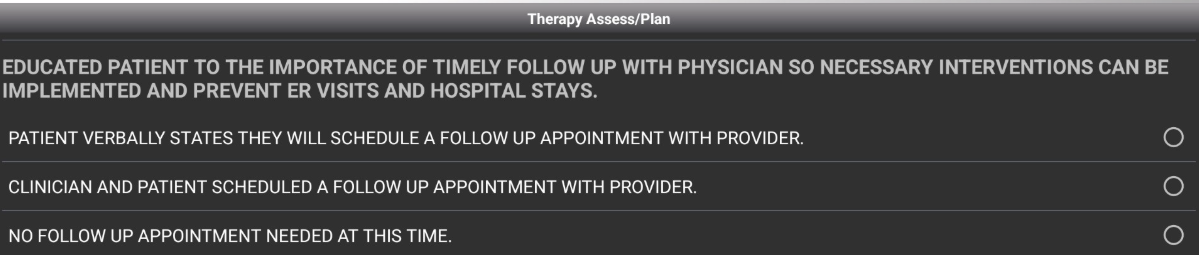
- Upon completion of this summary, a pick list will appear prompting POST DISCHARGE PATIENT/CAREGIVER INSTRUCTIONS/PLANS TO PREVENT HOSPITALIZATIONS AS ORDERED. Here the therapist will select all relevant discharge plans/instructions:
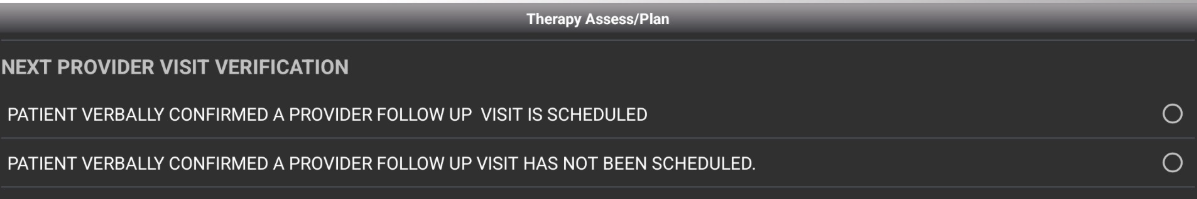
- 19 Service codes will end now. 18 service codes will have a pick list stating NEXT PROVIDER VISIT VERIFICATION. It is best practice for our patients to have a confirmed provider follow up visit following discharge from agency to best ensure continued positive clinical outcomes. The therapist will choose one of the 2 options:
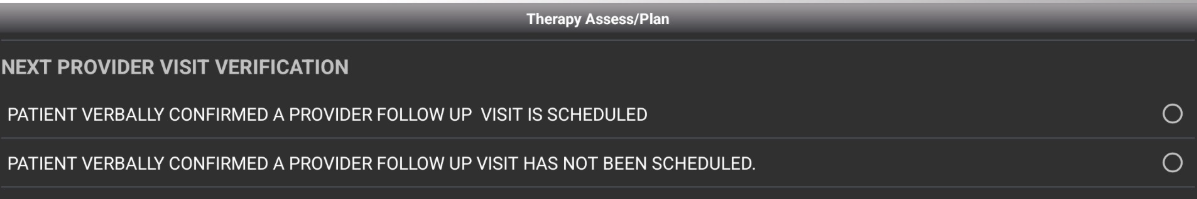
- If the second option 'PATIENT VERBALLY CONFIRMED A PROVIDER FOLLOW UP VISIT HAS NOT BEEN SCHEDULED' is selected, a second pick list will appear.