Policy:
Discharge, Transfer, Referral and Corresponding Summary https://aveanna.ellucid.com/documents/view/546
Purpose:
Guide clinician to complete a discharge summary that would need to sent to the primary care practitioner or other health care professional who will be responsible for providing care and services to the patient after discharge from the HHA (if any) within 5 business days of the patient’s discharge. Discharge Summaries will be added for each discipline during the discipline specific (19) visit type as well as the Agency Discharge discipline specific (18) visit type.
Regulation: G1022 §484.110(a)(6), G464 §484.50(d)(5)(i) , G598 §484.60(c)(3)(ii)
Measurement:
- 100% of chart audits will contain Discharge summary where appropriate
Process:
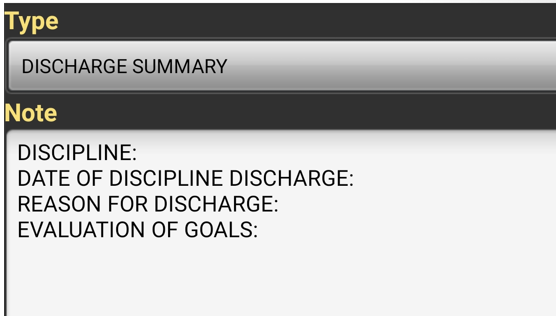
- Discharging clinician will add a note called Discharge Summary prior to completing the Discharge visit in Point Care.
- Discipline: Enter in the discipline that is performing the Discharge From agency Visit
- Date of the Discipline Discharge: Enter in the date of the discharge
- Reason for Discharge: Type in the reason why patient is being discharged
- Examples:
- Goals met
- Client no longer needs skilled services.
- Transitioning to outpatient setting for therapy
- Patient no longer homebound
- Examples:
- Evaluation of Goals:
- Describe patients outcomes and the goals that were agreed upon in the care plan.
NOTE: If client remains inpatient and certification period ends for current plan of care or discharges to another entity- Office will discharge chart. Clinician does not need to complete any further documentation.