Purpose:
To guide therapists on what to document in the Interventions/Goals section of an Evaluation visit.
Question Intent:
The Interventions/Goals section is intended to document the skilled interventions, techniques, strategies, and exercises that were addressed and instructed to patient/caregiver during the Assessment visit.
Per Medicare Benefit Policy Manual Chapter 7 - Home Health Services, the Interventions/Goals section highlights the importance “that the home health records for every visit will reflect the need for skilled medical care provided.”
Additionally, this guidance states, “the clinical notes are expected to tell the story of the patient’s achievements towards his/her goals as outlined in the Plan of Care”.
Response-Specific Instructions:
- At SOC (00) and Evaluation (01) visits, the therapist will click on Interventions/Goals to document their skilled interventions provided.
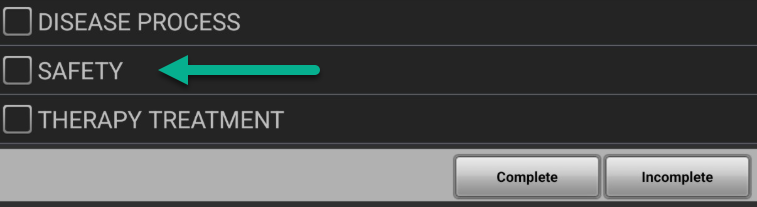
- Review the various categories in Interventions/Goals and proceed to document the skilled details and specific tasks that were addressed during that day’s Evaluation session. In this example, “Safety” is selected.
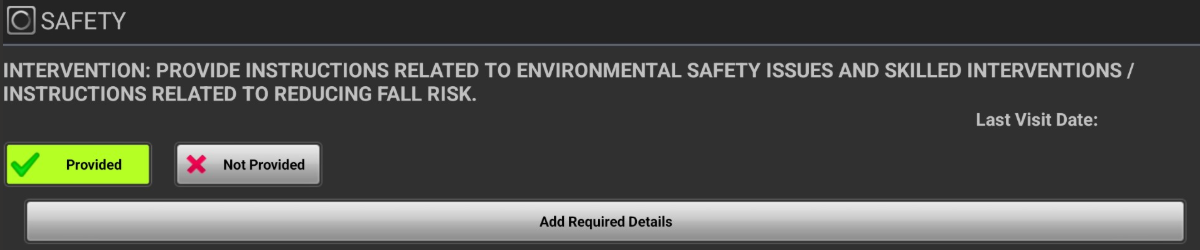
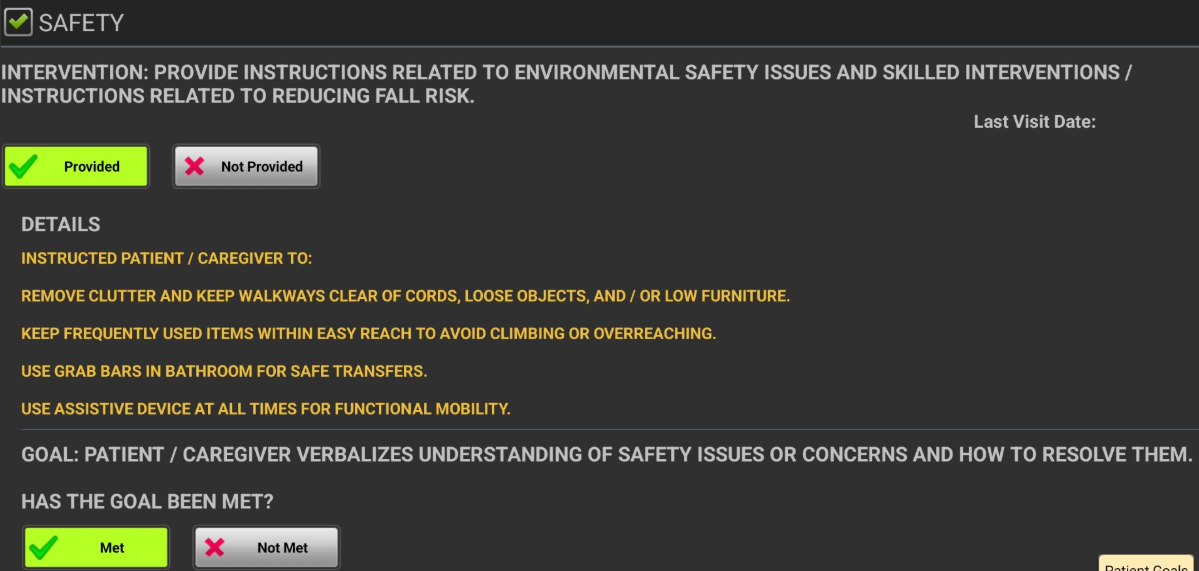
- To document that Interventions in this section were provided during the Evaluation, click on “Provided”, which will turn the button green.
- Then select “Add Required Details” to include specific details related to that category.
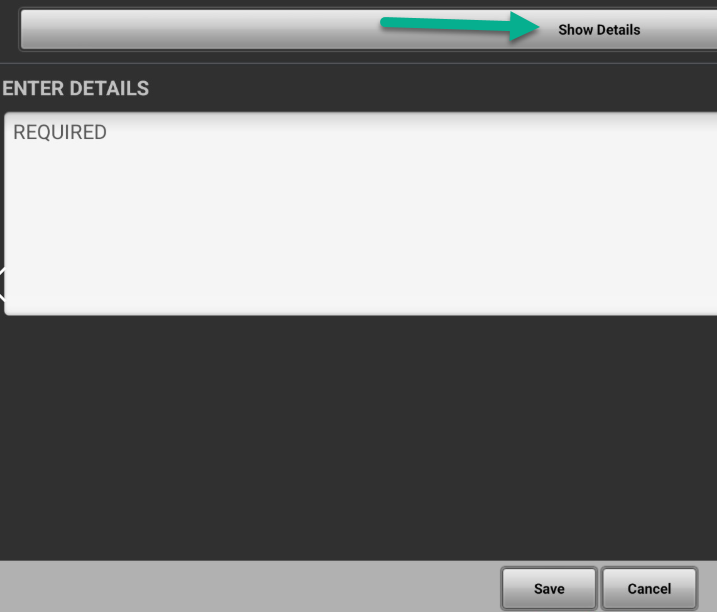
- Here the therapist will provide the appropriate details to document skilled interventions performed or instructed during the assessment visit.
- The therapist can either 'free text' their skilled intervention or can use the 'Show Details' option at the top of the screen to access a library of skilled interventions:
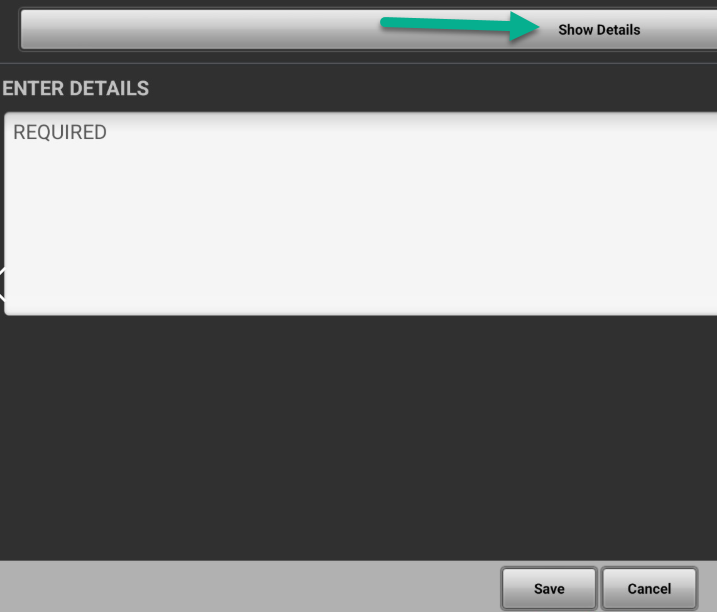
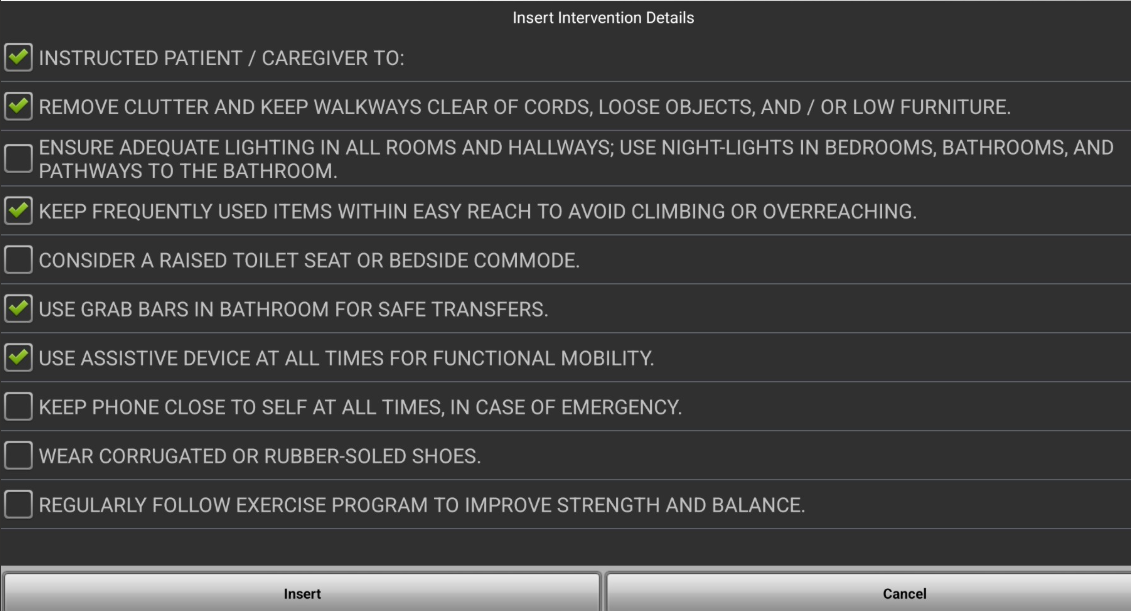
- Here is an example of 'Show Details' from the Safety Intervention, once chosen (green checkmark), the therapist can select 'Insert' to populate the free text area.
- Lastly, when an intervention is Provided, at assessment the therapist will ALWAYS choose the goal as Met. This follows a 'green - green' (Provided - Met) pattern to ensure that this intervention/goal falls off of the patient record and only future Interventions/Goals appear from 01 Pathways & New Order are documented to on future visits.
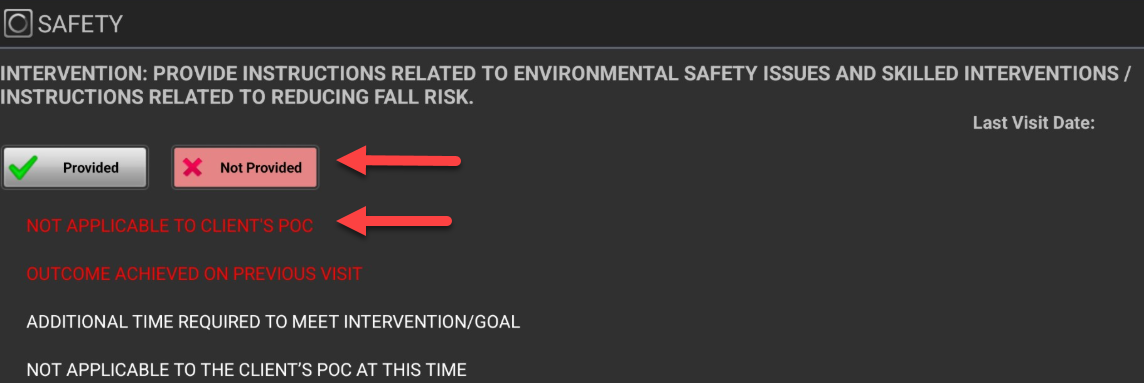
- At the Evaluation or SOC Visit, if the task is "Not Provided" be sure to select an option in RED which will ensure a 'red - red' (Not Provided - Not Applicable) pattern is followed so that this intervention does not proceed forward. This will ensure subsequent notes to not have irrelevant interventions and will also assist in avoiding duplicative documentation: